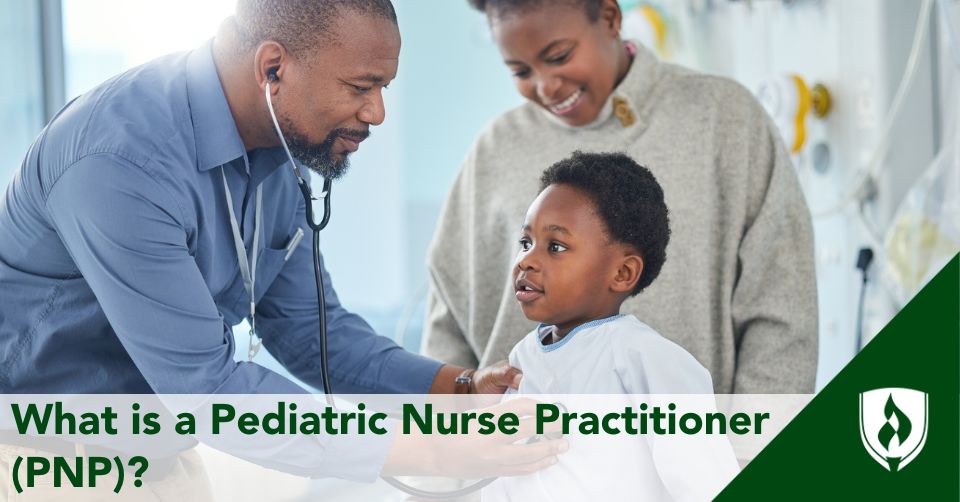
Pediatric nurse practitioners are specialized advanced practice nurses who deliver advanced nursing care to children. This includes children ranging from infancy to adolescents and young adults.
These practitioners obtain the necessary skills and expertise to assess, diagnose and manage the health care needs of children in various settings, while advocating optimal health via health promotion.
The advanced nurse practitioner's origin was born out of necessity in the mid 1960s in the United States. Its development was driven by the main factor of the growing shortage of primary care physicians. The pediatric specialization naturally became a priority, as there was a great need to improve overall access to children.
To help combat the increasing inaccessibility of quality care for children, advanced practice nurses established a pediatric care specialty. Since their incorporation over the years, pediatric nurse practitioners have been helping to alleviate the need for accessible child health services.
What are the duties of pediatric nurse practitioners?
The scope of your practice as a pediatric nurse practitioner is set (usually) by your state's board of nursing practice. This being said, there can be differences from state to state on the practice authority that is granted to you with your advanced practice nurse license.
Pediatric nurse practitioners are advanced practice nurses with usually a minimum educational level of a master's degree.
What makes these pediatric providers special is the unique approach they bring from their roots in nursing practice. From your training as a registered nurse, to your clinical hours working at the bedside, these experiences are what will make your patients love the care you provide.
Health promotion and preventive care
This is one of the most crucial functions the PNP is involved with-- administering well-child exams.
These are foundational aspects of pediatric care. These exams start around the birth of the child and proceed into their school years.
Well-child exams give children life-saving immunizations and check up on developmental milestones that should be met during these crucial years.
As the PNP, you will be educating not only the pediatric patients, but their parents and families as well. The education you will provide will focus on establishing and continuing proper health care promotion with adequate nutrition, hitting growth milestones and preventing disease.
Diagnosis and treatment plans
What makes pediatric nurse practitioners special is not only do they develop treatment plans like other healthcare providers, but they also bring a holistic approach to diagnosing and treating the patient.
As a pediatric nurse practitioner, you will be able to showcase your years of nursing experience to better assist your pediatric patient. You will have the authority to order diagnostic tests, order labs, and if needed, prescribe medications.
Pediatric patients will need your care for their acute and chronic health problems. You will be well-versed in ear infections, sore throats, asthma, diabetes, developmental disorders, and other common childhood illnesses.
The pediatric nurse practitioner is the "main manager" of care for the patient and thus will be in charge of coordinating care with other pediatric specialists when necessary. They can refer to therapists, pediatric cardiologists, gastroenterologists and psychiatrists (to name a few) as medically necessary.
Roles and settings for pediatric nurse practitioners
The pediatric nurse practitioner can be trained to work in various settings, including acute care (hospital), primary care (outpatient clinics), schools, and community health organizations.
Primary care settings
This is the original setting for most advanced practice nurses, and pediatrics is no different. Here, the PNP will handle the duties described above with the well-child exam at the center of their care.
This might look like a local clinic or other federally qualified health centers, and can include treating common pediatric acute illnesses, developmental screenings and general health maintenance to support optimal health in children.
Emergency departments
PNPs populate many pediatric emergency departments. I have seen several of my classmates from my family nurse practitioner program go straight into employment in the emergency room setting.
One of them was so intrigued by the pediatric emergency department, she even went back to complete her pediatric nurse practitioner specialization.
Urgent care facilities
Pediatric urgent care facilities have become more popular over the years. The majority are open throughout the day, and now I have also noticed urgent cares catering to late-evening hours as well.
School-based health centers
Children spend a great deal of their time in school. What better way to care for their health than with a school-based health center?
These healthcare facilities are located within or near a school and provide comprehensive medical, mental health and preventive care services to students.
These centers are designed to ensure that children and adolescents can easily access health services in a familiar and supportive environment, reducing barriers such as transportation issues, scheduling conflicts or lack of insurance.
Working as a nurse educator
So, you have spent years on the clinical side of things. You would like to take a break from the vaccines, scrapes, booboos and growing pains.
You are probably now a pediatric nurse practitioner pro and should go on to teach the future generations! As a resident physician, I love teaching nursing in my free time and continue to advance the profession that has given me so much.
Full practice authority vs. restricted practice for NPs
The scope of practice for pediatric nurse practitioners has evolved significantly over the past decade.
Currently, 27 states grant nurse practitioners (certified through the pediatric nursing certification board) "Full Practice Authority," allowing them to practice independently, without physician supervision.
In some states, nurse practitioners can practice independently immediately upon certification. Others require one to three years of direct supervision by a physician, before granting independence.
In contrast, 23 states mandate physician supervision for each certified pediatric nurse practitioner, referred to as "restricted practice." The specific requirements vary, but may include involving a physician in patient care, discussing treatment plans, or even requiring the physician to meet with some patients.
My home state of Florida is considered a "restrictive state." When I began practicing, I had a supervising physician, who reviewed and signed off on my patient charts as needed. Despite these restrictions, I found it manageable and appreciated having a collaborative relationship with another healthcare provider to ensure high-quality patient care.
The legal landscape for Nurse Practitioners continues to shift, often favoring greater autonomy. For example, after I transitioned to medical school, Florida passed legislation granting Nurse Practitioners autonomy in primary care. To obtain Full Practice Authority in Florida, PNPs must complete 3,000 supervised hours with an allopathic or osteopathic physician within five years.
Once these requirements are met, PNPs can apply to practice independently in primary care. Ultimately, whether under supervision or with Full Practice Authority, PNPs play a vital role in patient care, and the trend toward greater autonomy reflects the growing recognition of their contributions.
What does the path to becoming a PNP look like?
There are several routes to become a pediatric nurse practitioner. All require you to at least have an associate degree in nursing, as this is the minimal requirement to become a registered nurse.
After this, the most traditional way is to enroll in a science in nursing BSN and gain experience working in Pediatrics. Once you complete your BSN program at Rasmussen University, aim to get experience with pediatric nursing under your belt. For more on what that might be like, check out I Love Pediatric Nursing: Nurses Share What Makes It Worthwhile.
From there, you'll want to enroll in an Master's in Nursing - Nurse Practitioner (MSN-NP) program. After graduating, you will sit for pediatric nursing certification boards. The largest organization for the certification of nursing professions who provide care for children, adolescents, and young adults is The Pediatric Nursing Certification Board (PNCB®).
Why become a PNP?
The road to become a pediatric nurse practitioner is long--it takes a few rounds of education and lots of experience. But it's so worth it.
I can list so many reasons why you too should become an advanced practice nurse like me! As someone who obtained board-certification as a Family Nurse Practitioner, I had training in pediatric primary care and loved every second of it.
But, if I wanted to become more involved with their care, it would have been best to specialize in pediatrics, as this offers you more training and options to grow in the field.
Ask anyone who has worked with children in the healthcare field, and you will see--they tend to never leave. This patient population is something special and so rewarding. My life was forever changed, when I became a nurse practitioner.
To get more information on what this path requires, check out How to Become a Nurse Practitioner: Mapping Your Path.
PNCB® is a registered trademark of PEDIATRIC NURSING CERTIFICATION BOARD, INC.